Assessment 4 Instructions: Remote Collaboration and Evidence-Based Care
Create a 5-10 minute video of yourself, as a presenter, in which you will propose an evidence-based plan to improve the outcomes for a patient and examine how remote collaboration provided benefits or challenges to designing and delivering the care.
As technologies and the health care industry continue to evolve, remote care, diagnosis, and collaboration are becoming increasingly more regular methods by which nurses are expected to work. Learning the ways in which evidence-based models and care can help remote work produce better outcomes will become critical for success. Additionally, understanding how to leverage EBP principles in collaboration will be important in the success of institutions delivering quality, safe, and cost-effective care. It could also lead to better job satisfaction for those engaging in remote collaboration. Assessment 4 Instructions: Remote Collaboration and Evidence-Based Care
Demonstration of Proficiency
By successfully completing this assessment, you will demonstrate your proficiency in the course competencies through the following assessment scoring guide criteria:
· Competency 2: Analyze the relevance and potential effectiveness of evidence when making a decision.
1. Reflect on which evidence was most relevant and useful when making decisions regarding the care plan.
. Competency 3: Apply an evidence-based practice model to address a practice issue.
2. Explain the ways in which an EBP model was used to help develop the care plan.
. Competency 4: Plan care based on the best available evidence.
3. Propose an evidence-based care plan to improve the safety and outcomes for a patient.
. Competency 5: Apply professional, scholarly communication strategies to lead practice changes based on evidence.
4. Identify benefits and strategies to mitigate the challenges of interdisciplinary collaboration to plan care within the context of a remote team.
4. Communicate in a professional manner that is easily audible and uses proper grammar, including a reference list formatted in current APA style.
Professional Context
Remote care and diagnosis is a continuing and increasingly important method for nurses to help deliver care to patients to promote safety and enhance health outcomes. Understanding best EBPs and building competence in delivering nursing care to remote patients is a key competency for all nurses. Additionally, in some scenarios, while you may be delivering care in person you may be collaborating with a physician or other team members who are remote. Understanding the benefits and challenges of interdisciplinary collaboration is vital to developing effective communication strategies when coordinating care. So, being proficient at communicating and working with remote health care team members is also critical to delivering quality, evidence-base care. Assessment 4 Instructions: Remote Collaboration and Evidence-Based Care
Scenario
The Vila Health: Remote Collaboration on Evidence-Based Care simulation provide the context for this assessment.
Instructions
Before beginning this assessment, make sure you have worked through the following media:
. Vila Health: Remote Collaboration on Evidence-Based Care .
You may wish to review Selecting a model for evidence-based practice changes. [PDF] and Evidence-Based Practice Model s, which help explain the various evidence-based nursing models.
For this assessment, you are a presenter! You will create a 5–10-minute video using Kaltura or similar software. In the video:
. Propose an evidence-based care plan that you believe will improve the safety and outcomes of the patient in the Vila Health Remote Collaboration on Evidence-Based Care media scenario.
. Discuss the ways in which an EBP model and relevant evidence helped you to develop and make decision about the plan you proposed
. Wrap up your video by identifying the benefits of the remote collaboration in the scenario, as well as discuss strategies you found in the literature or best practices that could help mitigate or overcome one or more of the collaboration challenges you observed in the scenario.
Be sure you mention any articles, authors, and other relevant sources of evidence that helped inform your video. Important: You are required to submit an APA-formatted reference list of the sources you cited specifically in your video or used to inform your presentation.
The following media is an example learner submission in which the speaker successfully addresses all competencies in the assessment.
. Exemplar Kaltura Reflection .
9. Please note that the scenario that the speaker discusses in the exemplar is different from the Vila Health scenario you should be addressing in your video. So, the type of communication expected is being model, but the details related to the scenario in your submission will be different.
Make sure that your video addresses the following grading criteria:
. Propose an evidence-based care plan to improve the safety and outcomes for a patient based on the Vila Health Remote Collaboration on Evidence-Care media scenario.
. Explain the ways in which an EBP model was used to help develop the care plan.
. Reflect on which evidence was most relevant and useful when making decisions regarding the care plan.
. Identify benefits and strategies to mitigate the challenges of interdisciplinary collaboration to plan care within the context of a remote team.
. Communicate in a professional manner that is easily audible and uses proper grammar, including a reference list formatted in current APA style.
Refer to Using Kaltura [PDF] as needed to record and upload your video.
Note: If you require the use of assistive technology or alternative communication methods to participate in this activity, please contact DisabilityServices@Capella.edu to request accommodations. If, for some reason, you are unable to record a video, please contact your faculty member as soon as possible to explore options for completing the assessment.
Additional Requirements
Your assessment should meet the following requirements:
. Length of video: 5–10 minutes.
. References: Cite at least three professional or scholarly sources of evidence to support the assertions you make in your video. Include additional properly cited references as necessary to support your statements.
. APA reference page: Submit a correctly formatted APA reference page that shows all the sources you used to create and deliver your video. Be sure to format the reference page according to current APA style.
Remote Collaboration and Evidence-Based Care
Providing evidence-based care can be a challenge in any medical situation (Schmidt & Brown, 2017). However, it can be more challenging especially when the care is being provided remotely. Health care professionals should, therefore, collaborate with other health care personnel in different geographical regions to provide evidence-based quality care to patients who live in rural areas or have difficulties accessing a health care facility (Hardin, Kilian & Spykerman, 2017). This paper, therefore, discusses how health care professionals collaborate remotely and virtually to provide evidence-based care for patients.
Proposing an evidence-based care plan to improve the safety and outcomes for a patient based on the Vila Health Remote Collaboration
Evidence-based care plans provide nurses with important clinical information and best clinical practices that have greater potential to improve patient outcomes and minimize errors by standardizing the provision of care. Caitlyn visited Vila Health Facility and was diagnosed with cystic fibrosis. Cystic fibrosis is a type of genetic disorder. It occurs as a result of a mutation of the protein gene that is present in the body cells that secretes mucus. This particular protein gene is called cystic fibrosis transmembrane conductance regulator (CFTR). Cystic fibrosis primarily affects the gastrointestinal, reproductive and respiratory tracts.
Evidence based-care plans that are implemented should improve the safety and outcomes of patients. An evidence-based nursing care plan for patients with cystic fibrosis should include maintenance of adequate oxygenation, coming up with measures to eliminate pulmonary secretions, emphasizing the significance of adequate dietary and fluid intake, ensuring adequate nutrition, and preventing further complications.
Oxygen therapy should be administered to a patient. Supplemental oxygen will assist in maintaining adequate oxygenation. The work of breathing will be decreased. Calorie expenditure will also be reduced. The patient will then be relieved of dyspnea. This will increase comfort. The nurse administering care to Caitlyn should set a goal of maintaining the percentage of oxygen saturation to be higher than 90%. This is likely to translate to positive patient outcomes. Assessment 4 Instructions: Remote Collaboration and Evidence-Based Care
Several measures can be used to clear pulmonary secretions. The most common effective measure is administering airway clearance therapy to the patients. This will decrease the work of breathing and improve pulmonary function. Caitlyn will then be able to maintain an open and clear airway. This will result in normal depth and rate of respiration, normal breath sounds, and an airway that is free of pulmonary secretions, with a cough that is effective. If all these are achieved, then the patient safety and outcomes will have been enhanced.
It is also important for a nurse to ensure that the patient’s nutrition is adequate. The nurse should encourage the patient to take food that is nutritious. Adequate nutrition is likely to increase appetite and weight. The patient will also be free of signs or symptoms of mal-absorption. This will also translate to improved patient outcomes.
There are several ways in which a nurse can prevent complications of cystic fibrosis. The nurse can assess the patient’s knowledge concerning nutritional requirements, pathophysiology and genetics of the disease, and recommendations for controlling the infection. The patient should be able to verbalize the process of the disease, goals of therapy administered and treatment recommendations. This will finally result in improved patient safety and outcomes that is characterized by improvement in infection and suppression of bacterial growth. The cough will decrease and mucus production will shift to baseline. Positive patient outcomes will also be characterized by normal white blood cell count and normothermia.
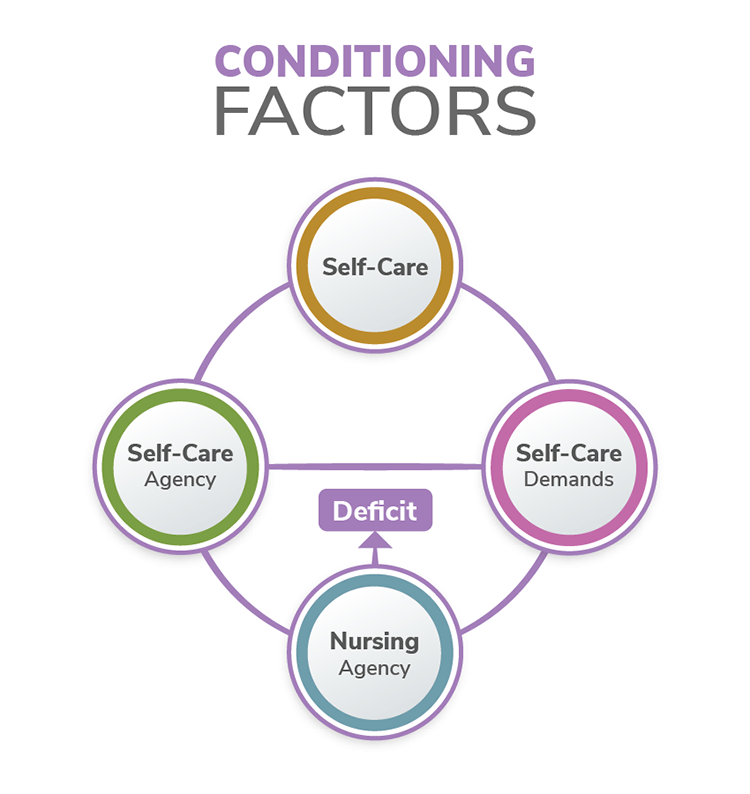
Explaining how an EBP model was used to help develop the care plan
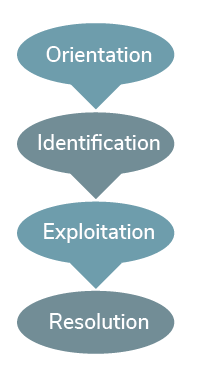
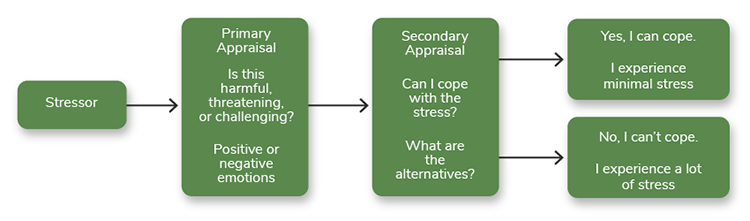
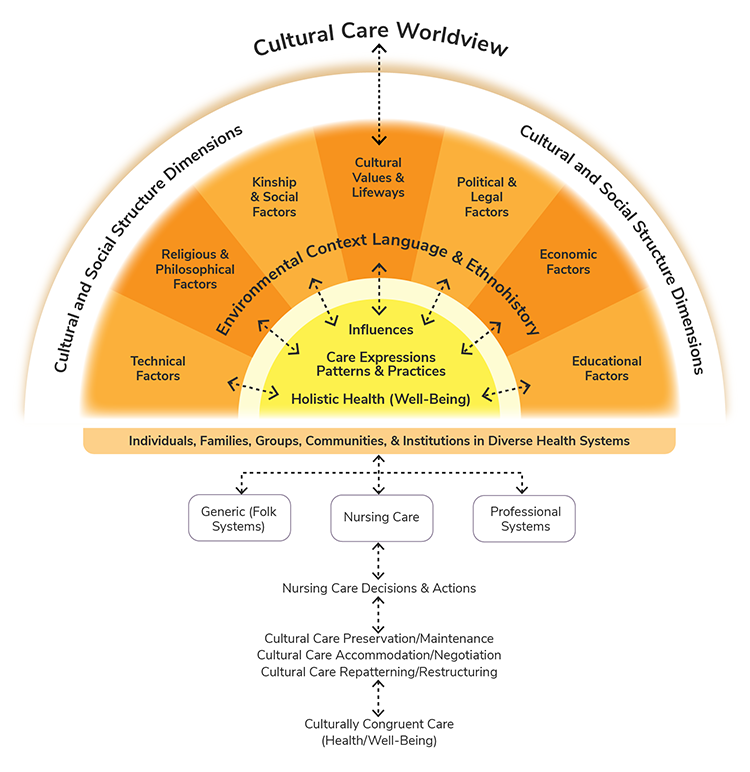
The Iowa Model for Evidence-Based Practice was used to help develop the care plan. This is because this particular evidence-based practice model helps in promoting quality care by ensuring the implementation of an evidence-based care plan. The model was used to develop the evidence-based care plan by better addressing the issue concerning patient-centric care for nurses at all practice levels and guiding them through a multiphase, collaborative and team-based process. The path starts with a clinical “trigger” that identifies a problem concerning the provision of care. It also includes decision points with evaluative feedback loops when suggesting and implementing a practice change about the provision of care. The Iowa model outlines the characteristics of a standardized evidence-based care plan that should be implemented by nurses in all clinical settings. The phases of the Iowa model include in are inter-professional team formation; review, critique and synthesis of evidence; implementation of the change via piloting; ongoing evaluation; and dissemination of results. All these processes were also used when proposing the evidence-based care plan.
The evidence that was most relevant and useful when making decisions regarding the care plan included positive results of patient-centered care, culturally competent care and patient education. These pieces of evidence informed the choice of the evidence-based care plans. This is because these pieces of evidence provided accurate and reliable information concerning how care plans can be used to improve the outcomes and safety of patients. The shreds of evidence also provided information on the care plan that is cost-effective.
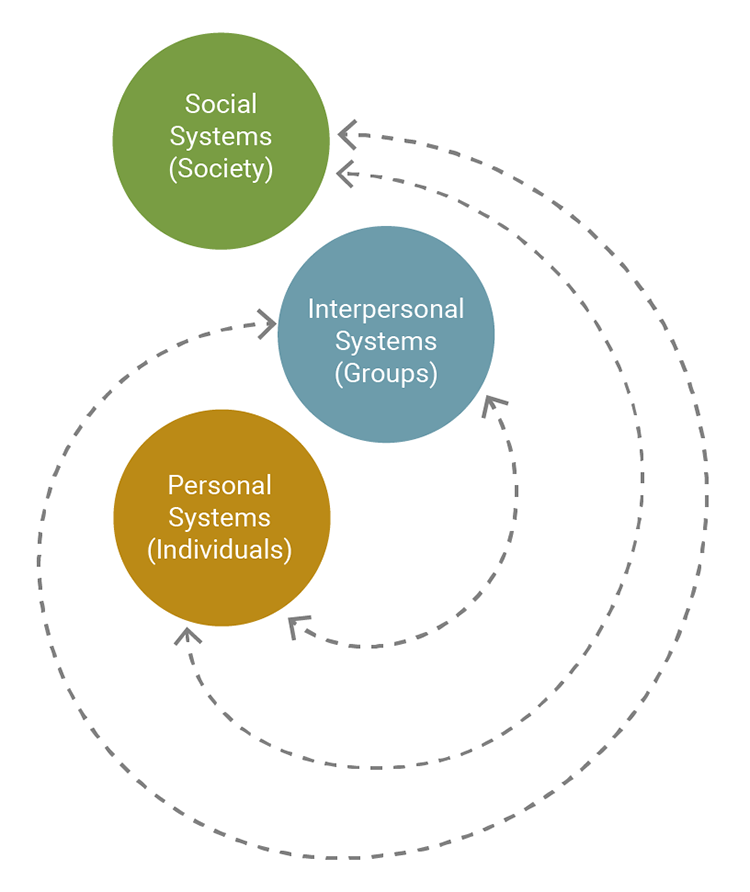
Identifying the benefits and strategies to mitigate the challenges of interdisciplinary collaboration to plan care within the context of a remote team
There are several benefits of interdisciplinary collaboration in remote settings. It leads to improvement in patient experiences and satisfaction. Medical errors are also reduced. This, in turn, improves the health outcomes of patients. Health care costs are also reduced. It also promotes coordination of care within the remote settings. Patients living in remote areas can access care.
There are various strategies to mitigate the challenges of interdisciplinary collaboration. Hierarchical structures that discourage interdisciplinary collaboration should be done away with (Supper et al., 2015). Professionals should be trained in interdisciplinary collaboration (Reeves et al., 2017). The interdisciplinary team should not be too large or too small. Interdisciplinary team members should be provided with enough resources as they work in remote areas. These resources can include financial resources and modern reliable technological equipment. The commitment of interdisciplinary collaborative team members should be emphasized. All these strategies are likely to mitigate the challenges faced by an interdisciplinary collaborative team tasked to work in remote areas. Assessment 4 Instructions: Remote Collaboration and Evidence-Based Care
Conclusion
Coordinating care can be challenging especially when a patient lives far from his/her care provider or when many health care providers are distant from each other. As discussed, nurses need to come up with evidence-based care plans. This is likely to quickly improve patient outcomes and safety. Modern technologies are necessary to provide quality evidence-based care to patients when care teams and patients are not in the same geographical location. Nurses and other health care personnel should develop creative solutions when challenges arise so that care planning for remote patients is as outcome-based and comprehensive as that for patients nearby or on-site.
Reflection Questions
How was remote collaboration used to improve the quality and safety of the care being provided in the scenario?
The patient was able to interact with a remote specialist and other health care providers via video-conferencing. The professional was able to remotely monitor the health status of the patient. The data obtained was used by the professional to suggest changes in a patient’s treatment and advise the patient to seek care. This resulted in an improvement in the safety and quality of the care being provided.
In what ways was evidence-based practice being effectively applied to help the patient in the scenario? Were there opportunities for improvement? If so, what were they?
The evidence-based practice was being effectively applied to help the patient in the scenario. EBP was used to keep the knowledge of the nurse up to date. This ensured that the nurse was able to deliver the care that is up to date. EBP was also used to enhance clinical judgment. The clinical decisions that were made by the health care professional were sound. EBP augmented the existing provider-patient decision-making process. The care provider-patient decision-making process was therefore made to be effective and efficient.
References
Hardin, L., Kilian, A., & Spykerman, K. (2017). Competing health care systems and complex patients: An inter-professional collaboration to improve outcomes and reduce health care costs. Journal of Interprofessional Education & Practice, 7, 5-10.
Lemberger, O., & Rossetti, J. (2018). An Integrative Review of Cross-Industry Global Innovation: Evidence-Based Strategies for Nursing Practice.
Reeves, S., Pelone, F., Harrison, R., Goldman, J., & Zwarenstein, M. (2017). Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews, (6).
Schmidt, N. A., & Brown, J. M. (2017). Evidence-based practice for nurses. Jones & Bartlett Learning.
Supper, I., Catala, O., Lustman, M., Chemla, C., Bourgueil, Y., & Letrilliart, L. (2015). Interprofessional collaboration in primary health care: a review of facilitators and barriers perceived by involved actors. Journal of Public Health, 37(4), 716-727.
Remote Collaboration and Evidence-Based Care
Evidence-based care can be a challenge in any medical situation, but particular challenges present themselves when care is being provided remotely. In order to provide quality care to patients who live in rural settings or have difficulty with transportation to a care site, health care professionals must sometimes collaborate with other professionals in different ZIP codes or even time zones.
In this activity, you will observe how health care professionals collaborate remotely and virtually to provide care for a patient in Valley City, North Dakota.
Valley City Regional Hospital
The Patient Presents
Dr. Erica Copeland and Virginia Anderson, a pediatric nurse, discuss Caitlynn, who came into the ER last night and has now been admitted to the pediatric unit.
Dr. Copeland and Nurse Anderson discuss Caitlynn, who came into the ER last night and has now been admitted to the pediatric unit.
Dr. Copeland starts the conversation.
Dr. Copeland: Nurse, can you give me an update on Caitlynn? I know she’s two years old and she’s been admitted for pneumonia. Does she have any history of breathing problems?
Virginia Anderson: Yes, this is her second admission for pneumonia in the last six months. She had a meconium ileus at birth.
Dr. Copeland: All right. Is she presenting with any other symptoms?
Virginia Anderson: She has decreased breath sounds at the right bases and rhonchi scattered in the upper lobes. Respirations are 32 and shallow with a temp of 101.
Dr. Copeland: What have we done for her so far?
Virginia Anderson: The respiratory therapist administered nebulized aerosol and chest physiotherapy. After the aerosol she had thick secretions.
Dr. Copeland: I see her weight is 20.7 pounds, and there’s been some decreased subcutaneous tissue observed in her extremities?
Virginia Anderson: Correct. I noticed this too, so she might have some malabsorption of nutrients.
Dr. Copeland: Have we done a sweat chloride test yet?
Virginia Anderson: Yes, and the results were 65 milliequivalents per liter. Also, the mother reports that when she kisses her, she tastes salty.
Dr. Copeland: All right. Well, I think it’s fair to say we might be dealing with cystic fibrosis here. Let’s get her started on an IV with piperacillin, and keep an eye on her temperature. Assessment 4 Instructions: Remote Collaboration and Evidence-Based Care
Collaboration Begins
Later, the diagnosis is confirmed: Caitlynn has cystic fibrosis. Dr. Copeland, Virginia Anderson, and Rebecca Helgo, the hospital’s respiratory therapist have a sort consult, where they realize that Caitlynn’s care will not be easy.
Dr. Copeland, Virginia Anderson, and Rebecca Helgo have a short consult.
Dr. Copeland starts the conversation.
Dr. Copeland: Let’s talk about Caitlynn Bergan. Her mother, uh, [checks notes] Janice, has been informed of her diagnosis. I didn’t realize this when she first came in, but she doesn’t live in Valley City; she’s in McHenry.
Rebecca Helgo: That’s a tough drive during winter. They’re over an hour away, aren’t they?
Dr. Copeland: That’s right. It was a toss-up between coming here or going to Jamestown, but I guess the father — Doug — thought Valley City was the better choice. Anyway, I’ve put her on Pancrease enzymes and we’ll be recommending a high-protein, extra-calorie diet along with the fat-soluble vitamins — A, D, E, and K. I’ll update her pediatrician on her condition, and order dornase alfa. Let’s see how she does with the breathing treatments. How are those going?
Rebecca Helgo: Quite well, actually. She’s too young to get her to do the huff breaths, but we’re keeping the secretions thin and manageable with the aerosol treatments. I am concerned about her day-to-day treatment, though. She’ll be back here with pneumonia if the parents can’t stay on top of that. She’s at risk for impaired gas exchange and respiratory distress, which will cause her anxiety and more distress, and that’s not going to help her stay well.
Dr. Copeland: How well do you think the parents will be able to handle the treatment?
Virginia Anderson: That might get tricky. I gather that the mother and father are still married but separated. We’ll need to make sure that at least one of them gets the education they need. But they both work, and trips here aren’t the easiest choice. We should get social services consult to coordinate services and identify some assistance for the family in McHenry.
Rebecca Helgo: I can do some education here, and then do a Skype consult with one or both of them once she’s been discharged and is back home.
Dr. Copeland: It sounded like both parents work long hours. Are you going to be able to schedule times that work?
Rebecca Helgo: I may have to do some after-hours appointments. We’ll have to sort that out.
Virginia Anderson: She’s had one bowel obstruction already, so I think we need to help them monitor for DIOS too. Does the pediatrician’s office have a telemedicine relationship with us? That might be helpful in preventing unnecessary trips here.
Dr. Copeland: Let’s find out a bit more and see what our options are. Assessment 4 Instructions: Remote Collaboration and Evidence-Based Care
Consulting With the Pediatrician
Later that day, Dr. Copeland and Virginia Anderson talk to Dr. Benjamin, Caitlynn’s pediatrician, about how his office can coordinate with the hospital on Caitlynn’s care
Dr. Copeland and Virginia Anderson talk to Dr. Benjamin about how his office can coordinate with the hospital on Caitlynn’s care.
Dr. Copeland greets Dr. Benjamin.
Dr. Copeland: Hello, Dr. Benjamin. I’m sorry to be meeting under such circumstances, but I hope we can work with you to help the Bergans handle Caitlynn’s care. On the line with me is Virginia Anderson, the nurse assigned to Caitlynn while she’s here.
Dr. Benjamin: Hello to both of you. Yes, it’s unfortunate. This is the first case I’ve seen among my own patients.
Dr. Copeland: Are you familiar with the CF protocol?
Dr. Benjamin: I am, but I’d love to get any more details that relate to Caitlynn. She’s done with most of her immunizations, but she’s still needs her HAV and influenza, of course. I’m also not sure where to order some of the pancreatic enzymes and medications you listed.
Virginia Anderson: We can help with all that. Do you have telemedicine access to Valley City?
Dr. Benjamin: No, but we do have it with Cooperstown Medical Center. We kind of have to in a town of less than 100 people.
Dr. Copeland: We may be able to use Skype on a more informal basis for consults between us, but it might be good to get connected with Valley City on your telemedicine equipment. If the parents bring Caitlynn to you with symptoms, and you’re not sure whether the hour-long trip is necessary, we can do a telemedicine appointment and make sure.
Dr. Benjamin: All right. It sounds like we might see them often initially, and I understand that bowel obstructions and pneumonia are two possible complications. We can handle some of those issues here, but assuming they have trouble during working hours, I assume we can reach you by phone?
Dr. Copeland: You or your staff can send me a text. If we need to talk further, we can set up a call, but if not, text is the quickest way to get my attention, and the easiest way for me to respond between things.
Virginia Anderson: And I’m available via text as well if you’re having trouble reaching Dr. Copeland or if it’s a question I can field.
The Care Plan Continues
To address some of the questions that came up during the consult, Virginia meets with Madeline Becker, the social worker at the clinic in McHenry.
Virginia and Marta Simmons meet with Madeline Becker, the social worker at the clinic in McHenry. Assessment 4 Instructions: Remote Collaboration and Evidence-Based Care
Virginia starts the conversation.
Virginia Anderson: Hi, Madeline, this is Virginia Anderson at Valley City Regional Hospital. I’m on the line with Marta Simmons, our social worker here at the hospital.
Madeline Becker: Hi, both of you.
Marta Simmons: Madeline, we’re calling because Virginia is working on a care plan for a child from McHenry, a Caitlynn Bergan. She’s here after a bout of pneumonia and she’s been diagnosed with cystic fibrosis. We wanted to talk to you about resources there for some of the issues the Bergans are going to be dealing with.
Madeline Becker: Of course. I got the documentation you emailed earlier. Fortunately, the Bergans are both employed and have good insurance through Doug’s new job. But as you may have heard, he was unemployed for some time, so money is tighter than it might seem.
Virginia Anderson: We’ve talked to Janice and she isn’t sure what her insurance covers as related to the breathing and other treatments Caitlynn is likely to need.
Madeline Becker: I can do some initial work on that. I’ll need a release from Janice to get detailed information, but I should be able to get general coverage information. What other resources might they need? McHenry is pretty small, as I’m sure you’re aware.
Marta Simmons: The main issue is going to be the stress of caring for a child with a chronic illness. Even a group that helps members deal with grief would be helpful. Children with CF live much longer than they used to, but it’s still a difficult condition.
Madeline Becker: There isn’t a group like that here, but there is one in Sheyenne. I mean, it’s more for parents in grief already, parents who have lost a child, but it’s a sizable group, relatively speaking. I’m sure there will be some parents who understand what it’s like to have a child with a difficult condition.
Virginia Anderson: All right, that helps. Now, we’re going to provide as much education as we can before Janice takes Caitlynn home, but what kind of resources are there in McHenry? If she doesn’t have home Internet access, does the library offer it? Is there a library?
Madeline Becker: No, the closest library is in Cooperstown.
Marta Simmons: Well, we’ll talk to the Bergans’ pediatrician and see if they might be able to help if they need materials and can’t get them easily at home. This is progressive and lifelong, and they’re going to need some support as they learn to deal with it.
Respiratory Therapist Consult on Skype
A few days after Janice an Caitlynn go back to McHenry, Janice calls to talk to someone about whether she’s doing Caitlynn’s chest physiotherapy correctly. Virginia and Rebecca, the respiratory therapist, call her back on Skype to answer her questions.
Virginia and Rebecca call Janice, on Skype, to answer her questions.
Virginia Anderson starts the conversation.
Virginia Anderson: Hi, Janice, thanks for contacting us! We’re getting back to you about Caitlynn. With me on the line is Rebecca Helgo, the respiratory therapist who helped you out when you were here.
Rebecca Helgo: Hi, Janice.
Janice: [sounding stressed] Hi.
Virginia Anderson: Janice, how is it going with Caitlynn?
Janice: Well, that’s why I called, actually. Not so good. I mean, not bad, but I guess I’m not remembering everything you told me when we practiced the physiotherapy, the chest physiotherapy.
Virginia Anderson: That’s okay, Janice. I know this feels overwhelming. Caitlynn’s condition is an extensive one, and we’re here to help you manage it. We’ll continue to be here as you’re figuring this out, okay?
Rebecca Helgo: That’s right, Janice. I know you’ll get the hang of it, but in the meantime there’s a lot to learn. So you had some questions about the chest physiotherapy? What’s going on?
Janice: Okay, if you can see on the camera, Caitlynn has these red marks on her ribs here. Is that a symptom of something?
Rebecca Helgo: Can you get the camera just a bit closer?
Janice: How’s that?
Rebecca Helgo: Okay, very good. Yes, those look like marks from the percussion. Are those over her last two ribs?
Janice: I think so.
Rebecca Helgo: That’s one thing you’ll have to remember: You don’t want to do the percussion on her last two ribs on either side, her backbone, or her breastbone. And when you do it anywhere else, you don’t want to leave red marks. So if you see those, that’s a hint that you’re doing the percussion just a bit too hard.
Virginia Anderson: Don’t worry, you haven’t hurt her that I can see. Plus, you’re obviously really staying on top of things and you’re following the recommended treatment procedures for Caitlynn, and I really want to praise you for that. So, is she acting like that area is hurting her? Or can you tell?
Janice: No, it doesn’t seem like it’s hurting her at all.
Rebecca Helgo: She should be fine, then.
Virginia Anderson: And remember, Janice, if you continue to have trouble with this, we’ve got other options. There’s a vest that vibrates the child if percussion isn’t getting the job done. And you won’t have to do exactly this forever. As she gets older and can learn how to do huff coughs, you’ll be doing less work and she’ll be doing more.
Janice: Okay. Thank you, that makes me feel better. I couldn’t get hold of my pediatrician and I was just getting worried.
Rebecca Helgo: Good, that’s what we’re here for.
Virginia Anderson: Janice, should we review the signs and symptoms of respiratory distress? We’re happy to go over anything you need to feel more confident about monitoring Caitlynn.
Janice: I think I remember those. I feel like I check for them every hour.
Rebecca Helgo: [chuckles] That’s understandable. Well, remember to check with Dr. Benjamin or me or Virginia if you need to. Assessment 4 Instructions: Remote Collaboration and Evidence-Based Care
Conclusion
Congratulations! You have completed this activity.
As you saw in this activity, coordinating care can be a challenge when the patient lives far from her provider or when multiple providers are distant from each other. Many technologies may be necessary in order to provide quality evidence-based care to patients when care teams and patients are not in the same location. Nurses and other health care professionals must find creative solutions when problems arise, so that care planning for remote patients is just as comprehensive and outcome-based as that for patients nearby or on site.
As you work on your assignment, consider these questions:
How was remote collaboration used to improve the quality and safety of the care being provided in the scenario?
In what ways was evidence-based practice being effectively applied to help the patient in the scenario? Were there opportunities for improvement? If so, what were they? Assessment 4 Instructions: Remote Collaboration and Evidence-Based Care


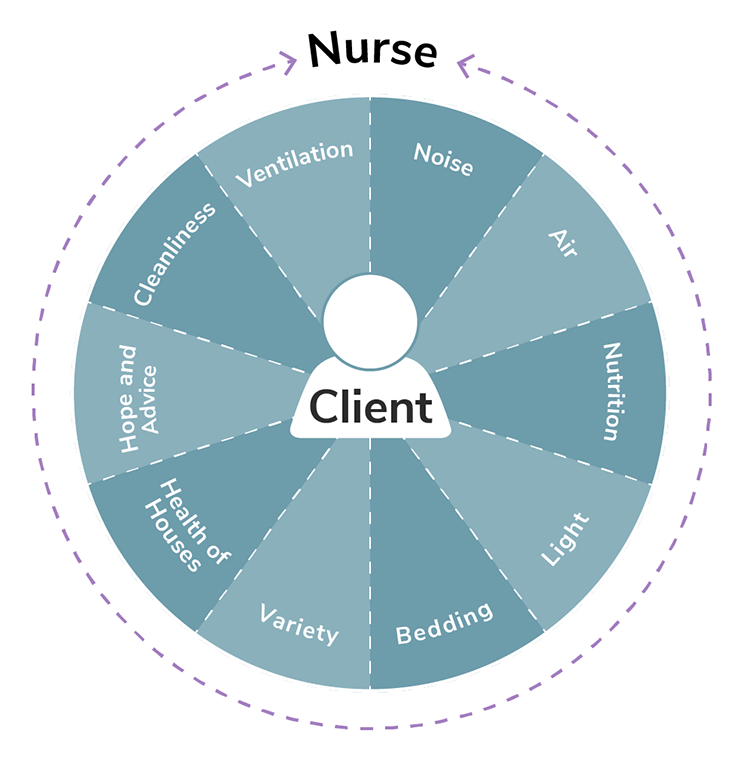
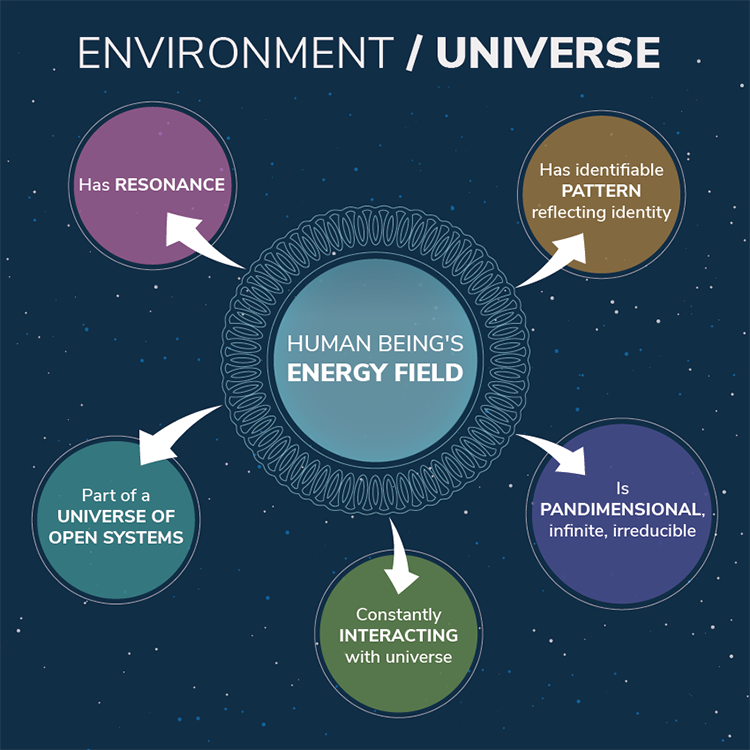 Example of Science of Unitary Human Beings TheoryA pediatric patient is hospitalized over the Christmas holiday. The patient’s mother, father, and two younger siblings are in the room as the nurse enters to assess the patient. The nurse feels that the atmosphere is very somber and wants to do something to improve the energy in the room. She mentions that she would be glad to bring in some Christmas DVDs if they are interested in watching movies. They agree, and when she enters the room an hour later, the family is laughing, enjoying a movie. The energy has changed in the room, and it feels more positive and cheerful.
Example of Science of Unitary Human Beings TheoryA pediatric patient is hospitalized over the Christmas holiday. The patient’s mother, father, and two younger siblings are in the room as the nurse enters to assess the patient. The nurse feels that the atmosphere is very somber and wants to do something to improve the energy in the room. She mentions that she would be glad to bring in some Christmas DVDs if they are interested in watching movies. They agree, and when she enters the room an hour later, the family is laughing, enjoying a movie. The energy has changed in the room, and it feels more positive and cheerful.